Bursitis is a general term for various painful complaints theorized or verified to be caused by inflammation of certain specialized structures common in many bodily joints, called bursa. These bursa are hollow sacs filled with synovial fluid, which is the liquid which enables smooth and frictionless joint movement. It is normal and expected for the joints of the body to degenerate with age and activity, therefore the loss of synovial fluid in the joints is a typical part of the aging process throughout the anatomy. In many cases, the symptoms implicated to be sourced from bursa degeneration are in reality caused by completely different structural or nonstructural processes. This fact helps provide evidence for why so many treatment options demonstrate poor curative results.
This investigational essay details why bursa inflammation might be a mistaken diagnostic theory when used to explain pain in multiple bodily locations.
What is Bursitis?
The bursa insulate muscles and tendons from their bony attachments. Imagine the bursa and the synovial fluid as being like oil in your car’s engine. The fluid helps to lubricate and prevent the buildup of heat and friction in the joint, just like oil does in the engine.
Remember that joints have moving parts which rub against each other during all activities and all this repetitive motion can create pain if the joint is not well protected. That being said, bursa inflammation is often misdiagnosed, since no swelling truly exists.
Although the pain may be theorized to come from bursa inflammation, some of these cases turn out to be tendonitis conditions, often linked to the psychosomatic process. Of course, serious structural bursa inflammation can exist and may be painful in rare instances. In these circumstances, the degree of degeneration and inflammation will be quite obvious.
When objective facts support structural pain, then that diagnosis is typically valid. However, diagnostic subjectivity often blames normal degenerative states unfairly for enacting symptoms when the joint changes are typical for the age and physical condition of the patient.
Causes of Bursa Pain
There is no known reason why some people suffer pain due to inflammation of the bursa, while others never experience any discomfort at all, even with comparable joint degeneration.
This occurrence is very similar to the incidence of pain theorized to stem from arthritis in the spine or degenerative disc disease, since these conditions are also virtually universal, but only create symptoms in some patients. This gives rise to the suspicion that many cases of pain with coincidental findings of bursa inflammation are indeed psychologically-induced, just like many cases of chronic back pain. Of course, patients who have lived a life full of particularly rigorous activities may suffer advanced deterioration of the joints which may be physically painful based on structural principles alone. However, this diagnosis is made incorrectly in many, many patients, explaining the often poor treatment results for bursa degeneration.
Finally, some patients also experience bursa-related pain from autoimmune disorders, such as rheumatoid arthritis, further adding credibility to the possible mindbody link, since many autoimmune concerns have been proven to be directed by the subconscious mind.
Bursitis Guidance
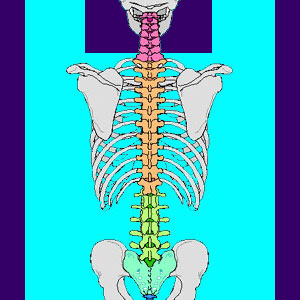
The most common areas to experience bursa-related pain are the hip, shoulder, knee and elbow, although the pain can occur in any synovial joint in the body, including the spine. We always warn patients who are diagnosed with bursa changes as their primary source of pain to research their diagnosis and compare their actual symptoms to those expected. There are often discrepancies, such as widespread pain which goes above and beyond the realm of specific joint movement or pain even when the joint is rested.
Additionally, there is also sometimes no evidence of actual inflammation, making the entire diagnosis suspect. In many of these cases, oxygen deprivation of the tendons is the actual source of pain and can sometimes be treated successful using knowledge therapy. This is certainly a better option than the risky pharmaceutical pain management which is typically recommended for bursa-related pain. At least there are no health risks with this alternative approach.
Back Pain > Psychologically Induced Pain Syndromes > Bursitis





